In the intricate realm of healthcare, proficient revenue cycle management (RCM) is crucial for maintaining financial stability and operational efficiency in medical practices.
RCM involves overseeing the entire patient revenue process, spanning from appointment scheduling to claim submission and reimbursement.
This blog delves into the complexities of revenue cycle management within medical billing, emphasizing its importance and offering a detailed, step-by-step analysis of the process.
Additionally, we will discuss strategies to enhance RCM and optimize revenue generation for medical practices.
What is Revenue Cycle Management (RCM) in Healthcare?
Revenue Cycle Management (RCM) is the systematic and coordinated approach to handling the financial aspects of patient care within healthcare organizations. It covers the complete journey of a patient’s engagement with the healthcare system, starting from appointment scheduling to the ultimate reimbursement of provided services.
In the nation of medical billing, Revenue Cycle Management involves essential elements such as patient registration, insurance verification, coding, claims submission, payment processing, and denial management.
An integral aspect of RCM involves communication with health insurance companies. Before a scheduled appointment, healthcare providers typically verify a patient’s reported insurance coverage. Following the treatment of an insured patient for a specific condition and the fulfillment of any applicable copayment, a healthcare provider or coder assigns the nature of the treatment using ICD-10 codes.
Later on, the care facility forwards a care summary, complete with ICD and Current Procedural Technology codes, to the patient’s insurance company to discover the coverage portion. After insurance coverage is determined, the patient is billed for the remaining amount.

Revenue Cycle Management (RCM): Essential for Successful Medical Billing
Effective revenue cycle management forms the cornerstone of prosperous medical billing and financial sustainability. Here are key reasons highlighting the importance of RCM for medical practices:
Enhanced Cash Flow:
RCM ensures the prompt and accurate submission of claims, facilitating quicker reimbursements. This enhances the cash flow for medical practices, enabling them to meet financial obligations promptly.
Reduced Billing Errors:
Robust RCM processes help healthcare organizations minimize errors in coding, documentation, and claim submission. This lowers the risk of claim denials, delays, and potential revenue loss.
Increased Revenue Generation:
Effective RCM maximizes revenue generation by identifying missed opportunities, optimizing reimbursement rates, and reducing billing and coding gaps that could lead to underpayments.
Improved Patient Satisfaction:
A streamlined RCM process enhances the patient experience by reducing billing-related issues, ensuring accurate and transparent billing, and providing timely resolution of payment queries.
The Benefits of Revenue Cycle Management
Efficient revenue cycle management ensures thorough and accurate steps to prevent delayed or lost revenue for providers. While the primary aim is to boost provider revenue, RCM also brings additional benefits, benefiting both providers and patients and enhancing the value of these processes. Let’s look at some of these benefits.
Identifying and Resolving Coding Errors
Implementing RCM helps providers easily spot errors in the medical billing process, reducing the chances of future denials, as around 90% of claim denials stem from preventable technical issues. These issues include missing patient chart information or incorrect coding.
Avoiding billing errors and gaining initial approval for claims accelerates reimbursement for providers, saving them from spending extra on investigating and appealing denied claims.
Reduced Administrative Complexity
Avoiding claim denials reduces the administrative burden. When administrative staff don’t need to invest time and effort in investigating and appealing denied claims, more resources are available for patient care.
RCM’s emphasis on front-end tasks also simplifies interactions between administrative staff and patients. Processes like appointment scheduling, intake form completion, claim submission, and medical billing are streamlined, contributing to a more satisfying experience for everyone involved.
Avoiding Healthcare Fraud
RCM provides a crucial benefit by preventing healthcare fraud and abuse, which costs the industry billions annually. Fraud investigations can jeopardize both revenue and reputation.
Inaccurate medical coding, whether intentional or not, can trigger fraud investigations. Common coding issues include billing for services not provided, medically unnecessary procedures, services by improperly supervised employees, and low-quality procedures or tests. Upcoding, where providers seek higher reimbursement rates for undeserving services, is another concern.
RCM’s focus on accurate data collection, medical billing, and coding reduces the likelihood of submitting incorrect information to insurance companies. It also keeps providers informed about evolving healthcare regulations, preventing unintentional fraud.
Increasing Healthcare Facility Revenue
By preventing technical errors, claim denials and fraud investigations, healthcare providers can quickly receive reimbursements for services. This helps avoid spending significant amounts on error resolution, claim appeals, and fraud investigations.
The additional revenue enables providers to invest more in patient care, aligning with their top priority of delivering quality healthcare.
Steps in Revenue Cycle Management
The revenue cycle management in medical billing typically comprises numerous interlinked steps, each integral to the overall financial well-being of a medical practice. Let’s delve into the details of each of these steps:
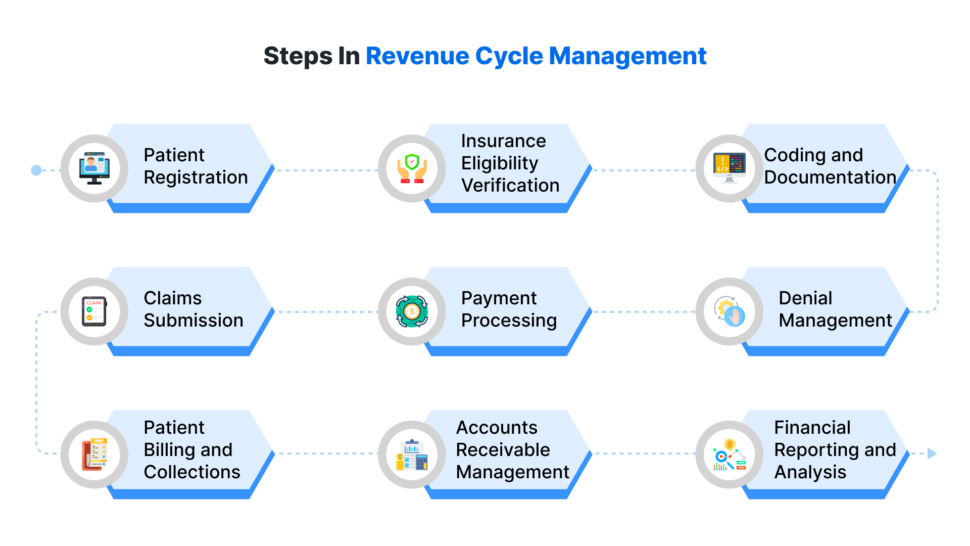
Patient Registration
The initial RCM step is patient registration. At this stage, essential details like patient demographics and insurance information are collected and input into the system. Accurate registration info is vital for seamless billing and claims processing.
Insurance Eligibility Verification
Before offering medical services, it’s crucial to check the patient’s insurance eligibility. This step confirms coverage under the insurance plan, identifying any potential payment issues.
Confirming insurance eligibility reduces claim rejections and minimizes financial surprises for both the patient and the healthcare provider.
Coding and Documentation
Precise medical coding is vital for getting the right reimbursement. Skilled coders assign codes to diagnoses, procedures, and services, translating them into a universal language for billing and claims. It’s important to have proper documentation supporting the chosen codes to ensure compliance and lower the risk of claim denials.
Claims Submission
After coding and documentation, claims are electronically submitted to insurance payers. The claims must meet payer requirements, including proper formatting and necessary supporting documents. Submission can be done through electronic data interchange (EDI) or clearinghouses, based on the payer’s preference.
Payment Processing
After getting the claims, insurance payers review and process them in a step called payment processing or claims adjudication. Payers check the claims for accuracy, medical necessity, and compliance with coverage policies. They decide the payment amount from the insurance payer and any patient responsibility like deductibles, co-payments, or co-insurance. Payments are received through electronic funds transfer (EFT) or checks.
Denial Management
Some claims might be denied or partially paid by the insurance payer due to reasons like incomplete documentation, coding errors, or lack of medical necessity. Denial management includes reviewing and analyzing denied claims to find the reasons. Healthcare organizations must then take appropriate actions, like resubmitting claims with more information or appealing denials when needed.
Effective denial management helps optimize revenue recovery and reduce revenue leakage.
Patient Billing and Collections
After the insurance payer decides the payable amount, the remaining balance or patient responsibility is billed to the patient. Patient billing involves creating and sending clear, itemized statements showing the services, insurance payments, and the patient’s financial responsibility.
Different payment options like online portals, credit card payments, or payment plans can be provided for quick and convenient collections.
Accounts Receivable Management
Managing accounts receivable includes keeping track of and monitoring payments due from both insurance payers and patients. Timely follow-up on unpaid claims and patient balances is crucial to optimize cash flow and minimize overdue accounts receivable. Regular analysis and reporting on the aging of accounts receivable help identify and address potential issues in the revenue cycle.
Financial Reporting and Analysis
During the RCM process, healthcare organizations need precise and thorough financial records. Financial reporting and analysis offer insights into overall revenue performance, identify trends, and aid in informed business decisions. Key performance indicators (KPIs) like collection rates, days in accounts receivable, and denial rates are tracked to gauge the financial health and operational efficiency of the organization.
By consistently and carefully following these steps, healthcare organizations can improve revenue generation, minimize claim denials, and secure financial stability in the constantly evolving field of medical billing.
How to enhance the RCM Process?
To improve the RCM process and boost financial results, medical practices can employ the following strategies:

Implementing Advanced Technology:
Integrating electronic health record (EHR) systems, practice management software, and billing automation tools streamline RCM processes, reduce manual errors, and enhance efficiency.
Staff Training and Knowledge:
Providing continuous training and education for RCM staff keeps them abreast of evolving regulations, coding guidelines, and payer requirements, minimizing errors and promoting accurate billing and coding practices.
Data Analytics and Reporting:
Utilizing data analytics tools helps identify trends, patterns, and areas for improvement in the revenue cycle. In-depth analysis of claims data and financial performance metrics supports informed decision-making and process enhancements.
Standardizing Processes and Optimizing Workflows:
Standardizing RCM processes and streamlining workflows eliminate redundancies, reduce errors, and enhance overall efficiency. Regular process audits and optimization support continuous improvement.
Patient Communication and Education:
Transparent and proactive communication with patients about billing processes, insurance coverage, and payment options builds trust and reduces confusion. Educating patients about their financial responsibilities ensures higher collection rates.
Compliance and Auditing:
Regular compliance audits, both internally and externally, ensure adherence to coding guidelines, billing regulations, and payer requirements. This minimizes the risk of fraud, penalties, and claim denials.
Outsourcing RCM Services:
Engaging specialized RCM service providers can alleviate the administrative burden and bring expertise in managing the revenue cycle. Outsourcing allows medical practices to focus on patient care while ensuring efficient billing processes.
Factors Affecting Revenue Cycle Management
Like all financial processes, revenue collection is influenced by both internal and external factors.
Collecting Payments From Patients
Patients are facing higher healthcare premiums. Collecting payments before or during their operation eliminates the risk of non-payment, though it can be challenging due to affordability issues and lack of awareness about financial responsibilities.
Patient pre-registration is vital to gather accurate medical history and insurance details upfront, preventing claim cancellations. This front-loaded approach includes obtaining information on insurance coverage, additional insurance, the patient’s minimum authorized visits, and establishing their financial liability.
Supervisory Processes are Factionalized
The front and back ends of the office may have conflicting priorities. Claim exclusions may happen without proper documentation. Clear communication about coverage suitability during patient intake can assist with payer integration, claims repayment, and payment enforcement.
Giving priority to front-end administrative tasks speeds up claims and helps less privileged patients understand their coverage options through insurance marketplaces. Patient insurance details are often overlooked on subsequent visits, leading to eligibility denials.
Eligibility Issues
Communication with private health insurers is crucial. Failing to follow up on insurance claims after filing can lead to delayed, denied, or rejected claims, including those that were never submitted. Monitoring claims to identify the root causes, such as issues with specific procedures or codes, helps raise awareness and prevent future occurrences.
Lack of Digital Workflow
Without the ability to simplify the technological process, there may be issues with poor-quality data and potential revenue cycle issues. Establishing a robust initial healthcare IT architecture supports RCM and the generation of necessary reports.
Introducing an interactive workflow can also facilitate the seamless coordination of front and back-office interactions and eliminate the loss of paper documents.
Conclusion
In summary, adopting effective revenue cycle management (RCM) processes is crucial for the success of medical practices in the dynamic healthcare environment. Key steps, such as investing in advanced technology, staff training, and outsourcing RCM services, contribute to achieving a smooth and efficient revenue cycle.
Managing each component of RCM can be challenging, and that’s where Ailoitte comes into play. Ailoitte offers top-notch Revenue Cycle Management services, assisting numerous healthcare systems in achieving significant growth in their medical billing and payment collections. Ailoitte’s RCM focuses on delivering excellent service, optimizing reimbursements, and providing valuable insights into your practice’s financial well-being
FAQs
The RCM process involves three primary stakeholders: the Patient, the Healthcare Provider, and the Healthcare Payer. Patients register at the hospital, receive treatment based on their insurance plan, and are reimbursed for their medical expenses.
End-to-end revenue cycle management (RCM) is a system for handling payments in healthcare services, covering everything from intake and billing to collections and reimbursement.
Essential principles of RCM involve identifying crucial assets, analyzing failure modes and effects, setting performance standards and thresholds, creating proactive maintenance strategies, and pursuing continuous improvement.
The medical billing process has several steps, and here are ten common ones:
1. Patient Registration
2. Insurance Eligibility Verification
3. Medical Coding
4. Charge Entry
5. Claim Submission
6. Payment Posting
7. Accounts Receivable Follow-up
8. Denial Management
9. Patient Billing
10. Reporting and Analysis
RCM workflows are the essential steps for a physician or healthcare organization to receive payment for the care they offer. These workflows involve tasks such as verifying eligibility, submitting claims, capturing payments, and managing denials.
Leave a Reply
Want to develop Revenue Cycle Management Software?
Get your software on time and within budget















.png)
.png)
.png)


Leave a Comment